Author: Rositsa Tashkova, Master of Molecular Biology and Microbiology
In recent years, reusable menstrual cups have become preferred by many women. They have many advantages over tampons and standard women's sanitary pads, among which in the first place may be environmental protection, since the cups do not generate the huge amount of non-recyclable waste unlike their "competitors".
Another advantage is that the collected matter in the cup is not exposed to oxygen and skin normal bacteria - unlike on the pads, which allows for a longer period of use of the cup within the day. It can stay in the body for up to 12 hours, while sanitary pads are changed every 4 hours so that they do not become a health risk.
What are the potential risks associated with the use of a menstrual cup
- Menstrual cups are made of silicone, but sometimes they also contain latex, so those allergic to this material should carefully read what the composition of their chosen cup is in order to prevent unwanted irritation.
- If the rules of excellent hand hygiene are not followed, both before the cup is inserted and the cup itself, its use runs the risk of infection. Just before the cup is used, it must have been thoroughly disinfected (by boiling before and after the menstrual cycle and by washing with soft, unflavoured soap on a water-based basis before and after insertion). Soaps containing oils are inappropriate. [ref. 1]
- Currently, there is only one described case of toxic shock syndrome (TSS) associated with the use of a menstrual cup. Toxic shock syndrome is usually associated with excessively long stay of a tampon in the body, which can lead to the entry of the Staphylococcus aureus bacterium, and sometimes those of the Streptococcus genus - normal inhabitants of the skin. The syndrome is potentially fatal, so it is extremely important to follow the instructions for use of tampons - they should not stay in the body longer than indicated, as well as not to use more absorbent tampons than necessary.
- In very rare cases, improper placement of the cup can affect the correct functions of other organs, such as the bladder, and the removal of the cup ceases symptoms. [ref. 7]
Endometriosis: do menstrual cups increase the risk
According to a 2003 report [ref. 2], the use of a menstrual cup may have caused endometriosis in a patient. This hypothesis has not been considered plausible by the regulatory authority (FDA - the US Food and Drug Administration) [ref. 3] and no other reports of a possible link between endometriosis and menstrual cups have been found to date.
In 2003, Dr. Armand Lione, president of the Association of Pharmacologists and Toxicologists, filed a petition with the U.S. Food and Drug Administration to revoke marketing approval for menstrual cups because he fears they are highly likely to cause endometriosis. The FDA's response is that there is not enough evidence to support this thesis. [ref. 4]
The introduction of the petition reads as follows:
"Menstrual cups, when used as currently recommended, can be worn for 12 hour periods during menstruation. They are designed to fit either over the cervix or within the vagina tightly enough so no menstrual debris is released from the body while a cup is in place.
Obstructions (blockage - b.c.) of the cervix and vagina are commonly recognized as important factors in inducing endometriosis. The cervical outlet obstruction inherent in the use of menstrual cups is likely to increase the incidence and severity of endometriosis among women who use these products."
Endometriosis is a disease in which endometrial tissue (normally building up the lining of the uterus, which falls off with any menstruation) appears in unusual places - ovaries, fallopian tubes, elsewhere in and rarely even outside the pelvic cavity. This tissue bleeds with any menstruation and causes severe pain.
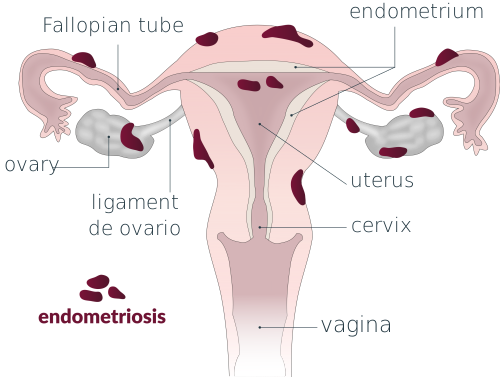
Since the causes of the disease have not yet been clarified, there are several theories about its occurrence. One of them states that peritoneal endometriosis develops when fragments of functional endometrium are released from the surface of the uterus during menstruation and returned back through the fallopian tubes (menstrual reflux) to reach the peritoneal (abdominal) cavity. Some endometrial fragments attach to the peritoneal surfaces, growing and degenerating cyclically, in connection with the menstrual cycle. These extra-uterine growths of the endometrium sometimes cause adhesions between peritoneal tissues and organs, causing very severe pain. When the tissues of the endometrium clog the ends of the uterine tubes, endometriosis can cause infertility. [ref. 5]
Dr. Lione also bases his concerns on this theory. He also writes:
"A clear distinction can be made between the blockage resulting from the use of menstrual cups and the occlusive potential of absorbent menstrual products such as tampons. [...] the tampon can retain the menstrual matter in its structure until its absorbent capacity is exceeded. When the tampon is saturated, it can also become an obstructive device, which would increase the reflux of endometrial tissues. However, the saturation of the tampon would also lead to leakage, which will also cause its removal from the vagina.
Unlike tampons, menstrual cups are composed of impermeable, non-absorbent materials. Menstrual materials retained in the cavity of the menstrual cup can easily return to the uterine cavity, as well as into the fallopian tubes and eventually to the peritoneum.
It should also be noted that clinical studies using menstrual cups show that the materials they collect contain viable endometrial cells. Although quantitative data on their effect on endometrial reflux have not yet been collected, it can be expected that a woman wearing a menstrual cup may inadvertently apply compression forces and stimulate endometrial reflux when occupying a number of routine poses that compress vaginal space or put pressure on the opening of the cervix." [ref. 4]
As we have said, there is currently no evidence to confirm Dr. Lione's concerns, but the question remains open to the scientific community for further research. In 2019, a review on the safety of menstrual cups has been published in the prestigious edition, and its conclusions are that menstrual cups appear to be a safe tool for now, but more qualitative research is needed on this relatively new product. [ref. 6]
