Author: Ivelina Yankova, Bachelor of Biomedical Sciences
What is marijuana?
Marijuana is derived from the Cannabis sativa plant, which was originally found in India and Central Asia. It has characteristic shaped leaves, gives flowering, which also has a characteristic appearance and can grow over three meters. Marijuana is the dried leaves, flowers, twigs and seeds of the plant. Cannabis contains over 120 active substances called cannabinoids or phytocannabinoids, the most famous of which are cannabidiol (CBD) and Δ9-tetrahydrocannabinol (THC).
How is marijuana used?
People most often smoke marijuana in paper in the form of a cigarette (joint), as well as in a pipe or water pipe (bong). Rolling it into a paper made of tobacco (blunt) is also a known method for use of the plant.
To avoid smoke inhalation, there are devices called vaporizers, which can also use liquid marijuana extract. They withdraw the active substances from the plant by decarboxylation (removing a carboxylic group from the compound, in which carbon dioxide is released – most often by heating) and storing their fumes in a specific part of the device. When smoking from the evaporator, these fumes are inhaled, which gives the same effect as when inhaling the smoke.
Also, the active substances can be extracted and mixed with various food products to prepare meals.
Lately, smoking or eating THC-rich marijuana extracts has become more common; these may be in a different form - oil, wax or solid.

Marijuana before and today
Marijuana use is believed to have started as early as 2900 BC. In the beginning, it was used for healing and there is evidence that the ancient Egyptians used it to treat glaucoma and inflammation of the body. In the original Jewish version of "Mass Exodus" (the second part of the Bible, which in Bulgaria we call the "New Testament") there are writings about sacred oil for anointing, in which content there was also marijuana. In 2900 BC, Chinese Emperor declared cannabis a popular drug and many other medicinal properties of this plant have since been discovered (ref.8).

The following records found were from 1000 BC, when Indians created a drink containing marijuana, which to this day is used as an anti-phlegmatic and anesthetic in India. Indians also believed that cannabis helps against dysentery and leprosy, a disease known in antiquity that was once considered incurable. Marijuana is known for its spiritual significance for the Indians. The notes of the ancient collection "The Vedas" claimed that cannabis was born from a drop of heavenly nectar that fell to the ground. This religiosity had spread cannabis use even further (ref.9).

Other ancient civilizations, such as the Greek, Roman, Arabic and English, have also used cannabis to treat various types of infections and diseases (arthritis, gout, syphilis, migraine, insomnia, etc.), and some had used it only for recreational purposes (ref.9). After the year 800, along with the spread of Islam, recreational cannabis use was on the rise because there was no specific ban on marijuana in the Koran.
As people's skills progress and due to the rapid growth and easy cultivation of marijuana, it begins to be used as a resource for making clothes, paper, ropes and sails for ships. Later, cannabis began to be used and grown by American colonies and by Spain during military missions.

By the mid-19th century, cannabis was already recommended by doctors and sold in pharmacies without the need for prescription (ref.10), and was even added to the American Pharmacopoeia, temporarily (ref.8).
It wasn't until the early 20th century that marijuana began to be used for recreational use in America when it was imported by Mexican immigrants into the country. This happened during the Mexican Revolution and the Great Depression in America, when there was mass unemployment. People are believed to have started hating Mexican immigrants and the marijuana they imported. The great misunderstandings led to the introduction of the "Marijuana Taxes Act" in 1937 – to be used only for specific industrial and medical purposes, only when paying excise duty (ref. 11).

Meanwhile, societies that opposed the ongoing change were growing. This continued until the late 1950s, when cannabis stopped being used entirely, and in 1970 President Richard Nixon repealed the Marijuana Tax Act and listed marijuana in the Controlled Substances Act as a first-degree drug, along with LSD, heroin and ecstasy. This law states marijuana as a drug with great potential for abuse and which has no medicinal properties that can be applied in medicine. This prohibition made it difficult to conduct any scientific research with the plant (ref.12).

Years later, despite the law's attempts to impose strict measures against marijuana, some states began to decriminalize its use for medical reasons, and by 2019, eleven states in America and other countries around the world legalize marijuana for both medical and recreational purposes.

The first research on the effects of marijuana
Nowadays, there are many studies done on the benefits and side effects of marijuana use. Moreover, we also know much more about the substances that are responsible for the properties of marijuana, medicinal or not.
The first published study on the healing properties of marijuana is from the year 1840 (ref.13). Dr. O'Shaughnessy first examined the effects of marijuana extract intake in animals, where he did not see any negative effects. Then he began clinical trials in people with different types of diseases – rheumatism, hydrophobia, cholera, dysentery, tetanus. In most patients, there were no noticeable improvements, but in the patients with tetanus, the doctor noticed significant improvements. Tetanus is a disease of the nervous system caused by the bacterium Clostridium tetani, which produces a toxin that affects the nervous system, causing painful muscle contractions all over the body. Dr. O'Shaughnessy believed that marijuana helped patients to cope with tetanus because it helps relax the muscles, which has led to a decrease in symptoms in these patients (ref.13). Subsequent studies have mentioned similar benefits of marijuana extract in diseases such as tuberculosis, rheumatism, tetanus, with the main and most notable effect being the relief of body aches that patients experience during diseases.
The cannabis plant produces 8 cannabinoid acids, from which the phytocannabinoids CBG, THC, CBD, CBC, CBGV, THCV, CBDV and CBCV are synthesized. These are the phytocannabinoids in marijuana that resound the plant with its interesting influences on our organism. Due to the rich information about the effects of these substances, here we will concentrate only on THC and CBD.
The two substances with the highest concentration in cannabis are Δ 9-tetrahydrocannabinol (THC) and cannabidiol (CBD). For the first time they were isolated from the plant in the 1940s, and their chemical structures were discovered in 1964 by Rafael Mekulam, who, a few years later, created the first synthetic cannabinoids (ref. 14), which to this day are used for scientific studies.
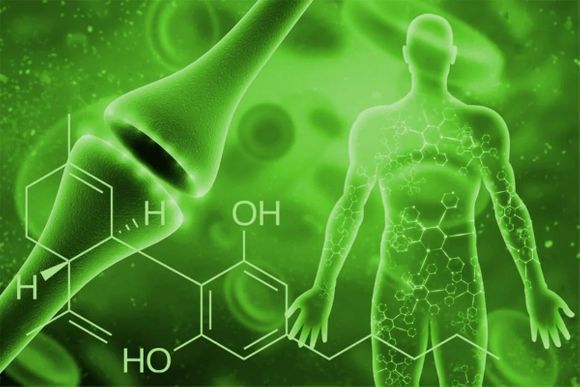
Phytocannabinoids express their properties mainly by binding to endogenous cannabinoid receptors. Such a receptor was first detected in 1988 (ref. 15), when phytocannabinoids were shown to bind to a specific substance in the membrane of cells and thus induce their specific actions in the body. To date, only two endocannabinoid receptors have been detected – CB1 and CB2.
Endocannabinoid system
Endocannabinoid receptors are part of a very important system for us called the endocannabinoid system (ECS). Its existence was discovered in the 1990s thanks to the inquisitiveness of scientists Allyn Howlett and Bill Devon and the new methods at the time in molecular science (ref.20). Not much is known about this system yet, but scientific studies have proven that it is important for the course of many processes that are essential for the normal function of the body. Some scientists believe that the role of ECS is to maintain homeostasis in the body.

In addition to the endocannabinoid receptors, a part of the ECS are endocannabinoids (two previously detected - anandamide (AEA) and 2-arachidonoylglycerol (2-AG)) and enzymes (amidy hydrolase of fatty acids and monoacylglycelic acid linase) whose role is to break down AEA and 2-AG when they are no longer needed.
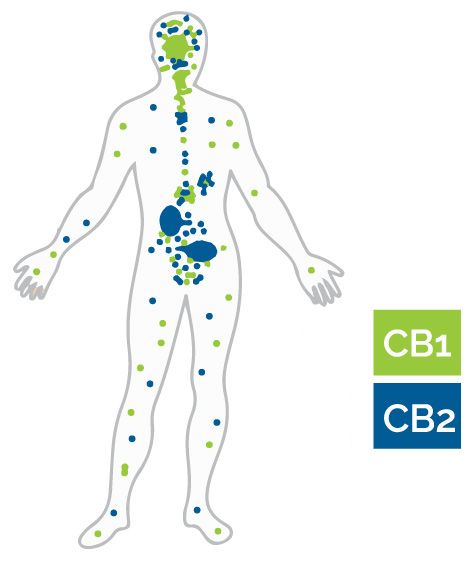
The majority of CB1 receptors are localized on the surface of nerve cells in the brain and more precisely in the anatomical parts, which are associated with cognitive impairment, memory, feelings of satisfaction, anxiety and pain, motor coordination and endocrine function. Also, a small part of CB1 receptors are located in areas of the peripheral nervous system - the spleen, white blood cells, endocrine glands, as well as in some parts of the reproductive, gastrointestinal and urinary system.
Unlike CB1, CB2 receptors are located mainly on the surface of cells in the peripheral nervous system – white blood cells, spleen and tonsils, and recently their presence was noticed in the central nervous system, but in a smaller concentration (ref.6).
How phytocannabinoids affect their actions
Phytocannabinoids are not part of the endocannabinoid system, but it has been found that their properties overlap to some extent with the properties of AEA and 2-AG.
CBD is one of the most studied phytocannabinoids due to its healing potential. Its effect on the body differs from that of THC, but it is believed that they may have a cumulative effect reinforcing the analgesic action of medical cannabis extract (ref. 17). CBD has a weak affinity (attraction) to CB1 and CB2 receptors, but in the presence of THC it may act as a CB1 antagonist (blocks the action of THC on CB1) and and a negative allosteric modulator of THC and AEA on the CB1 receptor (ref. 18, 19). This means that when CBD binds to CB1, THC's and AEA's affinity for that receptor is reduced, therefore reducing their effect in the body. It is believed that this property of CBD is key to its anti-inflammatory action, because when CB1 receptors are activated, the production of free radicals (these are oxygen-containing, highly reactive molecules that can cause chain chemical reactions in the body) and the pro-inflammatory substance TNF-alfa increase. Therefore, CBD's mechanism as a negative allosteric modulator reduces the activation of CB1 receptor (ref.31).
It is not yet known what the target of CBD is in the endocannabinoid system; some scientists believe that the receptor with which CBD binds has not yet been discovered. However, other CBD functions that are diverse in nature and most likely also play a role in the manifestation of CBD's healing properties have been found outside the ECS. One of its mechanisms of action is the binding to specific cation channels (TRP), leading to a decrease in the release of glutamate, which has the potential to lead to neural death if its levels are higher than normal (ref. 43). The antioxidant properties of CBD are exhibited in its ability to capture free radicals, interrupt the chain chemical reactions caused by them, and to model the action and levels of both antioxidants and oxidants (ref. 32).

THC is an analogue of the endocannabinoid AEA (ref.16) and gives the euphoric effect when using marijuana. THC has been shown to be a mixed agonist/antagonist of CB1 and CB2 receptors - it exhibits properties of both an antagonist and an agonist (the same as an antagonist, but instead of blocking, it mimics the properties of the substance it replaces) depending on the type of cell it binds to, the amount of receptors and whether there are endocannabionoids - complete agonists, that would replace THC (ref.7). Nevertheless, THC exhibits a strong affinity for the CB1 receptor, which is believed to be the cause of its psychoactive properties, as well as its potential proinflammatory properties.
In addition, THC can bind nonspecifically to other receptors in the body outside the ECS, as a result of which many of its known physiological properties are manifested. For example, it has been documented that THC affects the metabolism of certain proteins and nucleic acids (DNA and RNA) (ref.3), as well as of hormonal secretion and various neurotransmitters (ref. 4,5). Due to the wide variety of effects that THC has, no specific mechanism of action can be determined. THC exhibits analgesic, anti-inflammatory, antioxidant, antipruritic, bronchodilator, antispasmodic and muscle-relaxing properties. Also, it can also induce the production of free radicals (ref. 31, 35).
Diseases and symptoms in which positive effects have been observed
Multiple sclerosis
MS – multiple sclerosis – is one of the most commonly discussed diseases when talking about medicinal properties of cannabis. This is an autoimmune disease in which a person's own immune system begins to attack nerve cells. This causes typical symptoms - numbness of the palms and feet, loss of muscle tone and problems with balance, orientation and walking, fatigue and chronic pain in the body. In some studies, the effect of cannabis on some of the symptoms of MS has been proven, and it seems to improve them significantly. As early as 1987, in a clinical trial of MS patients an improvement in muscle tone (spasticity) was observed, which is often painful, after taking THC (ref. 28). In another study, two years later, similar results in spasticity and tremors in the muscles of MS patients were documented (ref. 29). In studies of animal models of MS, the muscle-relaxing and anti-inflammatory action of THC and CBD is observed. Unfortunately, the intake of a combination of THC and CBD by MS patients does not show as good a change as in animals, but compared to pre-existing MS drugs, the effect is similar (ref.30). In some countries, smoking medical marijuana, as well as use of synthetic cannabis drugs, is approved for MS patients as a cure for spasticity and pain that they experience (ref. 33).

Pain
We have all experienced the feeling of pain at some point in our lives - when falling from the bike or when touching the hot pan unintentionally. Unfortunately, there are people who experience it on a daily basis for one reason or another. This painful feeling is caused by nerve signals sent to the brain where they are registered, processed and finally perceived as a feeling of pain. Nerve cells that transmit this information to the brain have many cannabinoid receptors. Due to the effects that cannabinoids exhibit on these receptors, cannabis intake may block the registration of this information. For example, in a study on the effect of THC on patients with chronic and acute, non-chronic pain, a significant decrease in chronic pain was observed. Acute pain is not affected until a combination of THC and CBD is administered. This may be due to a combination of the effect as a negative allosteric modulator , which CBD exhibits to THC, along with the healing effects of CBD itself (ref.25, 26). In another study, it was seen that CB1 receptor levels are rising in patients with chronic pain, which may explain the analgesic action of THC in these patients (ref.27). In contrast to what we discussed until now, there are also studies that have shown the opposite effect - pain intensification, from taking marijuana, but only in acute non-chronic pain (ref.39).

Cancer
The most encouraging discovery about the effect of cannabinoids is on the effect they exhibit in cancer patients who are subjected to body aches all day. Cannabinoids have been shown to have a calming effect on this chronic pain in patients. In addition, in all patients in this study, and in many others, there was also a decrease in nausea and an improvement in appetite in these patients (ref.40). Due to mass monitoring of these effects, the Food and Drug Administration (FDA) approves THC (Dronabinol (Marinol®)) to treat nausea and vomiting, and to improve appetite in patients in chemotherapy (ref.41).
The same medicine is also approved in AIDS patients who experience similar symptoms.
There are scientific studies that show inhinition of tumor growth in patients in advanced stages (ref. 42), but more research in this direction is needed to prove this effect.
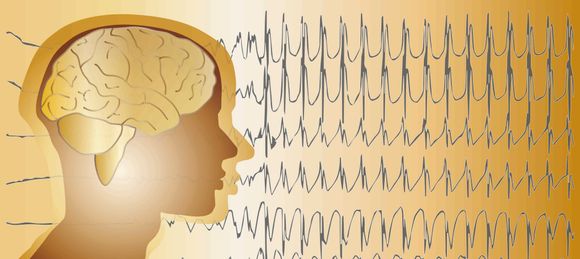
Epilepsy
Epilepsy is a common condition that affects the brain and causes frequent seizures. About a third of people with epilepsy are resistant to existing drugs (ref. 34). Various studies have shown a positive effect, specifically from taking CBD, for the treatment of seizures (ref. 37). Also, interesting is the cumulative effect of CBD with other antiepileptic drugs, as it seems that CBD increases their concentration, which in turn can improve results in these patients. This property is most likely the result of the inhibiting effect that CBD has on the P450 system (a large system of proteins that underpins drug interactions) (ref. 38). On June 25, 2018, the FDA approved a synthetic CBD drug (EPIDIOLEX) for the treatment of adults and children over 2 years of age (ref. 36). Although the permit is only for two specific epileptic syndromes, this is a great advance in the history of marijuana, as well as in the treatment of this disease.
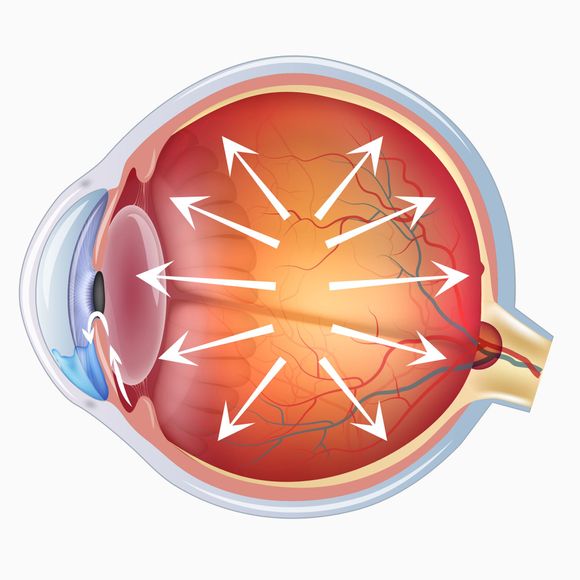
Glaucoma
One of the leading causes of blindness in the world is glaucoma. Glaucoma is a chronic disease in which the optic nerve that connects the eye to the brain is damaged. It is usually caused by a build-up of fluid in the front of the eye, which increases the pressure in the eye. There have been reports that smoking cannabis reduces eye pressure since 1970 (ref. 39). In subsequent years, this effect of cannabinoids has been demonstrated several times (ref. 44, 45). In addition, THC is considered a neuroprotective agent that can increase blood supply to the retina, aiding the survival of the eye nerve. Unfortunately, there are not enough studies on this issue to prove that phytocannabinoids are a good remedy for glaucoma.

Marijuana's benefits on other conditions
Cannabis intake seems to improve connections between different parts of the brain, but it also reduces the volume of this part in the brain associated with decision-making (ref 46).
There are many other benefits of cannabis use, such as constipation, skin problems, anxiety, etc.

Side Effects of Marijuana
Cognitive problems
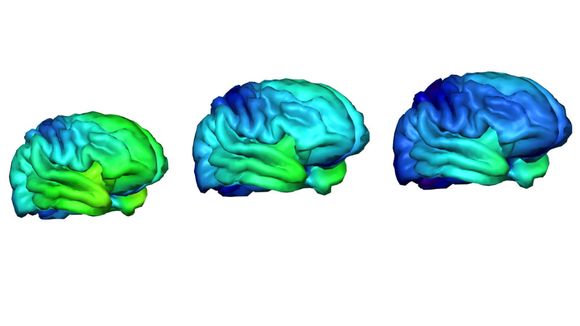
The harmful effects of taking marijuana are most often caused by long-term use, especially in teenage years. A series of studies have proven that chronic cannabis use leads to cognitive brain damage – it becomes difficult for the abuser to concentrate, remember and learn new things, as well as to make simple decisions (ref.46, 47). Over the years, persistent memory and attention disorders increase (ref. 48); and the difference between long-term and shorter cannabis use in these indicators is significant (ref. 49). These cognitive changes in the brain may resume after a long period of abstinence (ref. 51).
Chance of psychosis
Numerous studies have analysed the possibility of psychosis in people using cannabis and in most, if not all, a link between the two occurences has been proven (ref. 50).
One reason for the onset of psychosis in people using cannabis may be that THC causes neuronal noise - random neural activity in the brain.

Occurrence of chronic bronchitis
Smoking marijuana is also associated with more frequent occurrence of chronic bronchitis, since the smoke that is inhaled can promote inflammation of the lungs, increased airway resistance and pulmonary hyperinflation (ref. 52).

Propensity to dependency
Last but not least, repeated cannabis use can lead to addiction – about 30% of people who use marijuana develop a form of addiction (ref. 53), with children under 18 much more likely to develop dependence than older people. Fortunately, it is almost impossible to overdose with marijuana, but other symptoms such as increased heart rate, headache and panic attack may occur with too much use (ref. 55).
ABCD study
As the brain develops most rapidly in adolescence, in 2015, scientists created a national study (Adolescent Brain Cognitive Development℠ Study (ABCD Study)), in which they observe the development of the different parts of the brain of 10,000 9-10-year-olds for the period of 10 years. The scientists hope that the data collected by the participants will create baseline standards for typical brain development. The study will also monitor changes in children who use cannabis (ref. 54).